Highlight 11/2023 – WHO Emergency care system framework
Juan Camilo León Pamplona, 15 March 2023
Emergency care is one of the many health topics that the World Health Organization (“WHO”) addresses as a part of its mandate. More precisely, emergency care is defined by the WHO as an essential part of the health system and serves as the first point of contact for many around the world. This first point of contact is relevant and critical in scenarios where there are logistical or financial barriers to healthcare access and/or when people are symptomatic with acute illness or injury independently of their age and the nature of the emergency, injury and/or disease. As a result, emergency care aims at prioritizing an integrated approach to early recognition and to reduce morbidity and mortality correlated to the above-mentioned illnesses and injuries.
In this context, the emergency care system framework surges as one of the eleven (11) tools devised by the WHO to aid emergency care in achieving its objectives. The main goal of this framework points towards assisting policy-makers that evaluate and desire to strengthen national emergency care systems. The WHO emergency care system framework is a result of global debates between policy-makers and emergency care providers around the world gathered to discuss the capacity of the framework, plan and fund priorities and establish monitoring and evaluation strategies.
Thus, the above-mentioned framework intends to directly address core emergency care functions when dealing with injury or illness, expressly related from transport to emergency unit and early inpatient care. Consequently, the assessment varies depending on the available resources each State holds and allocates for this area. In short, the WHO emergency care system framework allows policy-makers to deploy the essential system functions to analyze where current and future gaps exist in order to propose and execute action plans to develop these context-relevant priorities.
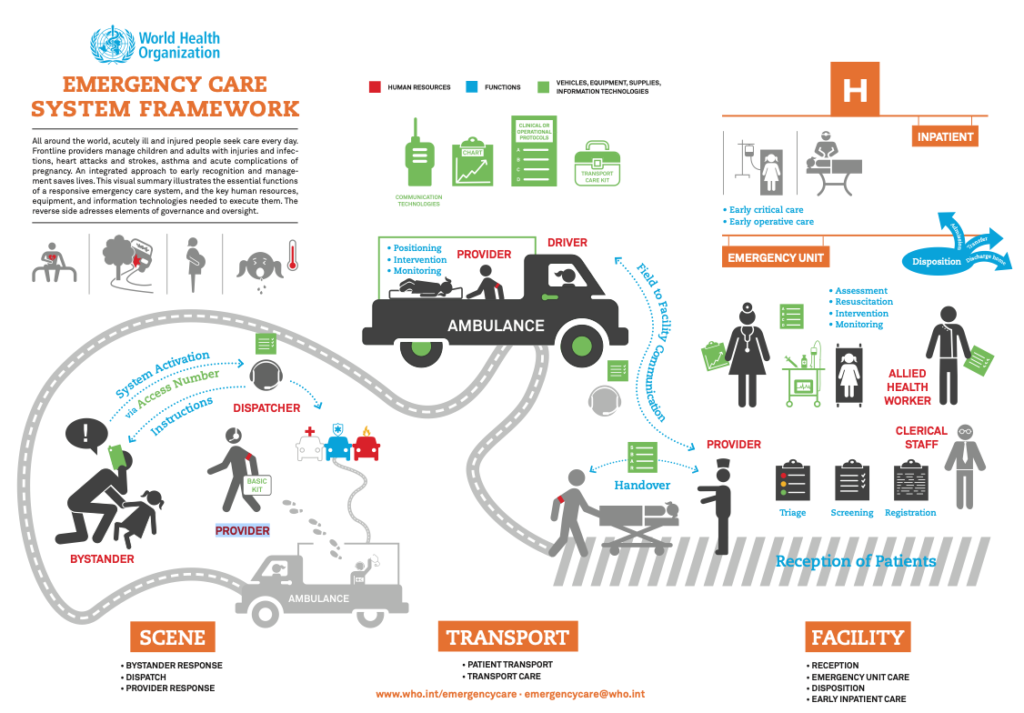
According to the WHO emergency care system framework, the identified core functions of the system are: system activation from a bystander to a dispatcher, instructions from the dispatcher to the bystander and information to the ambulance, police, and/or firefighters; positioning, intervention and monitoring by the ambulance provided to the patient, handover from the ambulance provider to the reception of patients provider; mutual communication between the ambulance driver and the reception of patients provider; triage, screening and registration of the patient by the clinical staff; assessment, resuscitation, intervention and monitoring from health care workers; and finally disposition (admission, transfer or discharge home) by the health care workers. Nevertheless, when dissecting the framework, several issues arise related to the viability and the possible challenges in the implementation.
On the one hand, concerning the viability, the WHO emergency care system framework highlights human resources, equipment and information technologies as key variables that support the efficient and effective functioning of a responsive emergency care system. On the one side, regarding human resources, the framework underlines roles such as bystanders, ambulance basic kit providers, dispatchers, ambulance driver, reception of patients provider, allied health worker and clinical staff. On the other side, when inspecting equipment and information technologies, the WHO emergency care system framework emphasizes items such as an access number so the bystander can contact the dispatcher to activate the system and then receive information as to how to deal with the patient, basic kits from the ambulance provider to attend the patient, ambulances (equipped with transport care kit, clinical or operational protocols, charts and communication technologies) to transport the patient to be handed over to the reception of patients provider and ultimately charts, protocols and specialized medical equipment that are handed over from the ambulance provider to the reception of patients provider and further treat the patient.
On the other hand, with regards to the implementation, the framework also distinguishes vital control and governance elements such as accreditation of equipment and services to ensure quality and safety, systems protocols that provided guidance for critical processes, certification of providers to ensure compliance with training standards and, lastly, key time intervals to be used as process metrics to better understand the performance of the system.
Accordingly, despite WHO’s emergency care system framework ambition, existing and potential challenges to the viability and the implementation of the framework persist and may deepen in specific countries due to availability of resources and diverse priorities. Initially, to develop the needed human resources, not only specific education is needed but also allocation of resources by the State and private sectors (depending on the nature of the medical facility) to (re)build the staff, deepen expertise and consolidate the network. Afterwards, the equipment needed also demands resource allocation from the Government which would signify cutting funding from other crucial sectors. Finally, both the human resources, equipment and governance/control elements, constantly need to be modernized and improved to fit international standards, which also implies constant investment to update the care architecture.
Juan Camilo León Pamplona, Highlight 11/2023 – WHO Emergency care system framework, 15 March 2023, available at www.meig.ch
The views expressed in the MEIG Highlights are personal to the authors and neither reflect the positions of the MEIG Programme nor those of the University of Geneva.
